By
Rebekah Urbonya
 I have severe gastroparesis and intestinal dysmotility. In early 2014, I was given my first feeding tube, a nasojejunal (NJ) tube. My medical team and I had a difficult time finding a formula that I could tolerate. When we finally did, a gastrostomy-jejunostomy (G-J) tube was surgically placed in my abdomen. But soon
after, my gastroparesis and intestinal dysmotility worsened, and despite many interventions, I stopped tolerating tube feedings. I had signs and symptoms of malabsorption, was unable to eat or drink fluids at all and became drastically underweight. Dehydration
and malnutrition became urgent issues and prompted a 2-month stay in the hospital.
I have severe gastroparesis and intestinal dysmotility. In early 2014, I was given my first feeding tube, a nasojejunal (NJ) tube. My medical team and I had a difficult time finding a formula that I could tolerate. When we finally did, a gastrostomy-jejunostomy (G-J) tube was surgically placed in my abdomen. But soon
after, my gastroparesis and intestinal dysmotility worsened, and despite many interventions, I stopped tolerating tube feedings. I had signs and symptoms of malabsorption, was unable to eat or drink fluids at all and became drastically underweight. Dehydration
and malnutrition became urgent issues and prompted a 2-month stay in the hospital.
That summer, after seemingly exhausting all options, I was started on parenteral nutrition (PN) to deliver nutrients intravenously through a central line. The adjustment to PN was overwhelming. There is a big learning curve in transitioning to IV nutrition and managing care for a central venous catheter in the home
setting. My support system—patient advocates, friends, family, and a team of health professionals, has been essential in helping me cope with long-term home parenteral nutrition (HPN) and the medical complications that may arise. But not only had PN help me regain some health stability, it also saved my life.
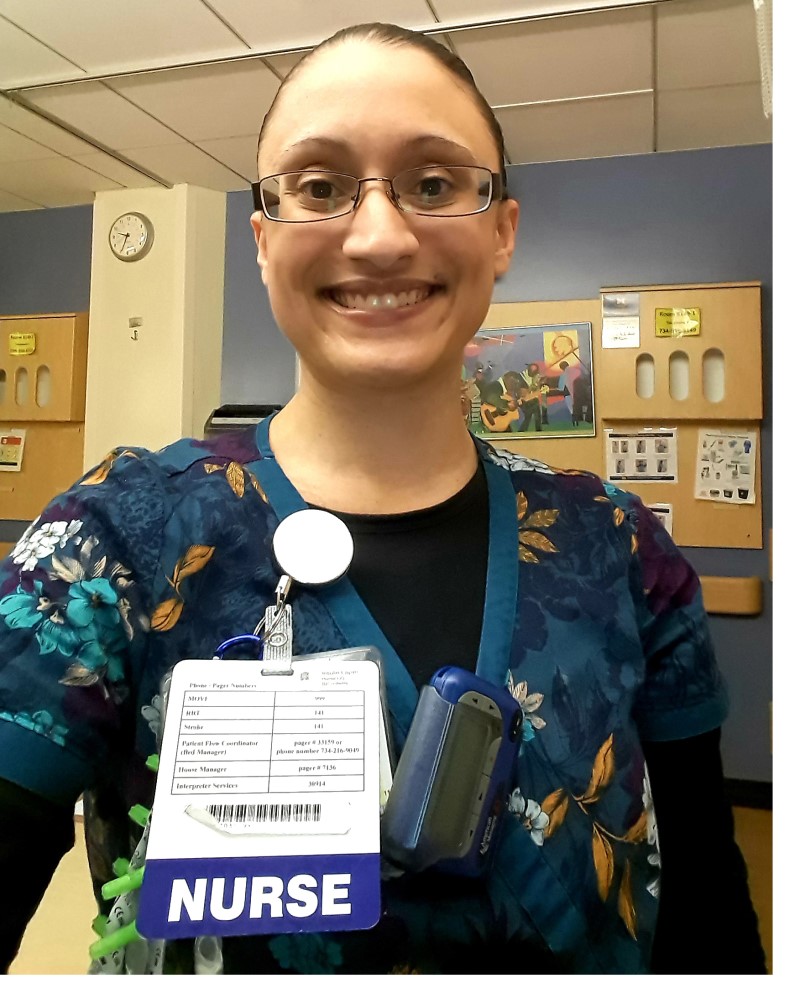
Eventually, I resumed my part-time position as a clinical research coordinator. To help me keep moving forward, I remained involved in meaningful activities and set realistic goals. One of my early goals was to attend a yoga class once per week—and I accomplished that! Obtaining a nursing degree was a long-term goal
that I set prior to the significant decline in my health, and I still wanted to fulfill that dream. I took college courses to meet the prerequisites for the program, and when the acceptance offer came, I went for it! I conquered many health obstacles
throughout school, including a hospitalization from sepsis due to a crack in my central line. However, I remained resilient and graduated at the top of my nursing class.
Today, I work as a registered nurse on an adult inpatient general medicine unit. Due to my 20-hour PN cycle, I infuse while at work. I use a fanny pack to carry my infusion pump and PN bag. I find it works better than a backpack. I infuse IV fluids for hydration before and/or after work, in addition to pushing oral
hydration through my G-J tube as much as tolerable. Nutrition support is literally the fuel providing 100% of my nutritional needs and makes it possible to carry out my passion for nursing.
Managing long-term HPN is very much a team effort, and my gratitude goes out to the providers and staff—“Team PN”—who make these medical therapies possible. As a complex patient, my personal experiences strengthen my ability to professionally advocate for patients’ needs and, alongside a team of knowledgeable clinicians,
help me provide patient education on interventions, including nutrition support. Our collective efforts share the common goal of promoting positive patient outcomes.
Read more patient stories.